Whiplash Imaging: What Radiology Can and Can’t Explain
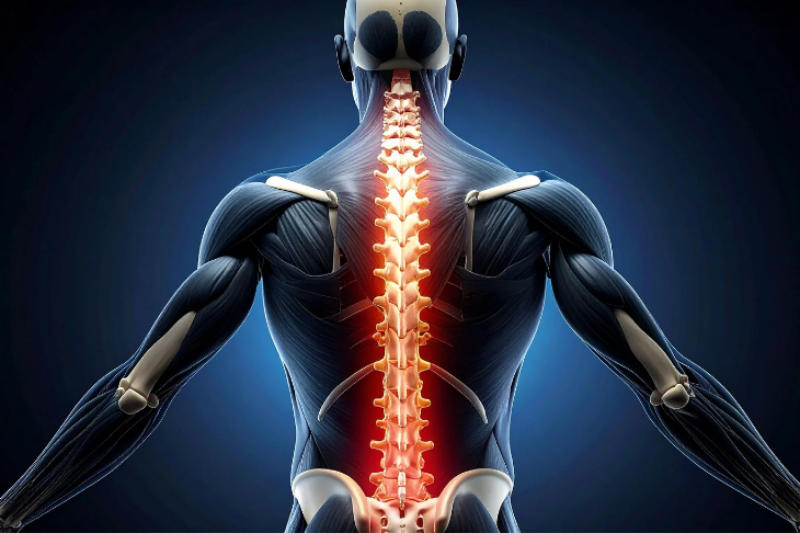
Traditional imaging often fails to detect whiplash injuries. Even with "normal" MRI and CT scans, a significant portion—up to 80%—of soft-tissue and micro-structural damage from whiplash is missed, as confirmed by 2025 clinical studies. This explains why half of whiplash patients don't fully recover despite having "clean" scans. Modern neuro-diagnostics have evolved to focus on functional imaging and objective oculo-vestibular testing to better identify the underlying cause of persistent symptoms.
Board-certified physicians
Objective, FDA-approved testing
Multidisciplinary concussion rehab
What 2025 Research Changed About Whiplash Imaging
A "normal" MRI does not mean you aren't injured. 2025 clinical studies confirm that standard MRI and CT scans miss up to 80% of the soft-tissue and micro-structural damage caused by whiplash. Modern neuro-diagnostics have shifted toward functional imaging and objective oculo-vestibular testing to explain why 50% of whiplash patients never fully recover despite "clean" scans.
What Clinicians Should Do Differently
- Acknowledge the "Invisible" Lesion: Understand that standard 1.5T or 3T MRIs lack the resolution to see microscopic axonal shearing or facet joint capsule tears. Stop using "Normal MRI" as a reason to discharge symptomatic patients.
- Utilize Upright/Kinetic Imaging: 2025 protocols suggest using Weight-Bearing (Upright) MRI or Digital Motion X-ray (DMX) to visualize ligamentous laxity that disappears when a patient is lying flat in a traditional tube.
- Correlate with Neuropsychology: If imaging is silent, look to Neuropsychological Evaluations (NPE). Cognitive "slow-down" is an objective marker of brain network dysfunction that no standard MRI can visualize.
What Patients Should Know
- The "Picture" vs. The "Function": An MRI is a still photo of your anatomy; it doesn't show how your nervous system is functioning. You can have a perfect-looking engine that won't start—your brain is the same way.
- 40% Have Symptoms 30 Years Later: Research shows that 40% of whiplash survivors still have "nuisance" symptoms decades later because the initial microscopic damage was never properly addressed.
- Facet Joints are the Culprit: About 25% of chronic whiplash pain comes from the facet joints or discs—structures that are notoriously difficult to assess on standard radiology.
Frequently Asked Questions (FAQ)
Q1: My MRI was normal, so why does my neck still hurt?
A: Standard MRIs look for "gross" issues like herniated discs or broken bones. They cannot see the microscopic tears in ligaments or the "stretching" of nerves that occurs during a high-speed whiplash event.
Q2: What is the best test for whiplash if an MRI is clear?
A: Objective functional testing, such as Vestibular-Ocular Reflex (VOR) testing or a Neuropsychological Evaluation, can provide data-driven proof of injury where radiology fails.
Q3: Can whiplash cause a brain injury?
A: Yes. The "whip" of the neck often causes the brain to strike the inside of the skull (coup-contrecoup), leading to a mild TBI that is rarely visible on a standard CT scan.
Q4: Is "Whiplash" just a muscle strain?
A: No. While muscles are involved, chronic pain is usually rooted in the facet joints, spinal ligaments, or the central nervous system's "pain volume" being turned up too high.
Q5: How does All Things Neuro document whiplash for legal cases?
A: We use a "Whole Person" approach, combining clinical examination with objective testing to create a defensible record of impairment that doesn't rely solely on radiology.
Next Steps
Don't let a "normal" test result stop your recovery. If you are still in pain, your injury is real—it's just invisible to outdated technology.
Schedule an Objective Diagnostic Evaluation
Wellness Disclaimer
This content is intended to support education and awareness around health and wellness topics and does not replace personalized medical care. Whiplash and associated disorders are complex; readers are encouraged to consult with the specialists at All Things Neuro to determine the appropriate diagnostic path for their specific injury.
.gif)